Division Spotlight: Metabolism, Endocrinology and Nutrition
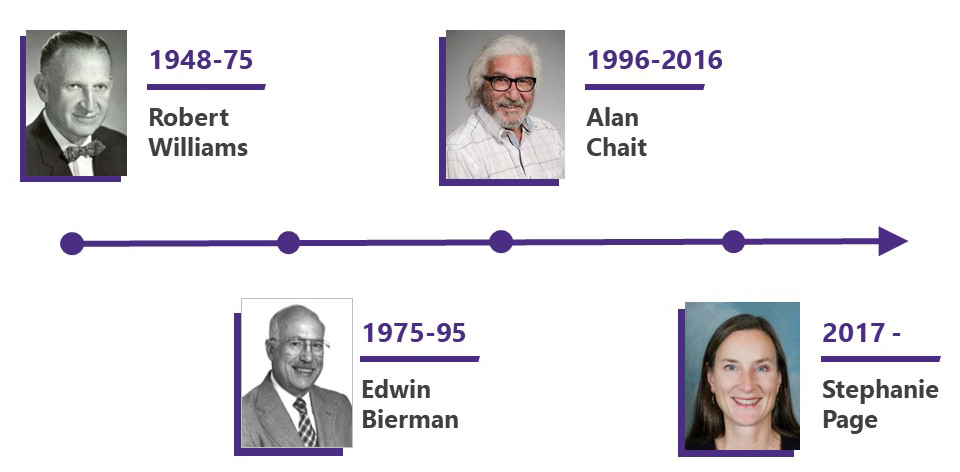
 In 1948, Dr. Robert H. Williams, a nationally prominent endocrinologist, was appointed to chair the newly established Department of Medicine at the University of Washington School of Medicine.
In 1948, Dr. Robert H. Williams, a nationally prominent endocrinologist, was appointed to chair the newly established Department of Medicine at the University of Washington School of Medicine.
Celebrating 75 years
As part of our 75th Anniversary, we plan to spotlight each of our divisions over the course of the year, in the order that they were established. Learn more about our 75th Anniversary on our website.
He founded the Division of Endocrinology - the department's first subspecialty division - the same year and headed the division and was chair of the Department of Medicine from 1948-1963. He continued as division head until 1975. In 1978, the division name was changed from Endocrinology to its present name.
Our faculty have a long and distinguished history of cutting-edge research, spanning the range from basic science research, through clinical investigation; state-of-the-art innovative clinical care; and first-rate teaching. The spirit of excellence continues today, with outstanding education, clinical, and research programs.
EDUCATION AND FELLOWSHIP TRAINING
We are dedicated to training the next generation of physicians and scientists in the areas of diabetes, endocrinology, metabolism, and nutrition.
Our Endocrinology fellowship program offers two training tracks to provide fellows with educational and practical experiences to prepare them for their intended careers: a two-year clinical scholar track for physicians interested in academic or community-based clinical practice, and a three-year research track for physicians interested in a more extensive research experience, with aspirations for an academic research career or career in industry.
The UW Medicine Diabetes Institute (UWMDI) trains postdoctoral fellows interested in investigating the causes and consequences of obesity, diabetes, and related metabolic and vascular disorders.
Many of our trainees have gone on to academic careers in endocrinology and hold leadership positions in both academia and industry.
PATIENT CARE
We provide a full spectrum of clinical care for our patients through compassionate community-based and innovative subspecialty clinical locations.
 The UW Diabetes Care Center (now part of the UW Medicine Diabetes Institute) opened to patients in 1991 and was a showcase for the institution. It was one of the largest sites in the landmark Diabetes Control and Complications Trial, to study glucose control as a way to reduce the microvascular complications of type 1 diabetes.
The UW Diabetes Care Center (now part of the UW Medicine Diabetes Institute) opened to patients in 1991 and was a showcase for the institution. It was one of the largest sites in the landmark Diabetes Control and Complications Trial, to study glucose control as a way to reduce the microvascular complications of type 1 diabetes.
 The UW Medicine Diabetes Institute was founded in 2019, creating a “bench to bedside” institute dedicated to advancing the understanding and treatment of diabetes and its complications.
The UW Medicine Diabetes Institute was founded in 2019, creating a “bench to bedside” institute dedicated to advancing the understanding and treatment of diabetes and its complications.
Basic scientists, a clinical research unit, and a multidisciplinary team of clinicians are co-housed to facilitate collaboration and accelerate work toward both prevention and a cure for diabetes.
The Diabetes Care Center nearly doubled its patient volumes in the first 2 years and continues to partner with other divisions, including Nephrology and Cardiology, in providing comprehensive care for our patients with diabetes.
Subspecialty care
Comprehensive Pituitary Program
The Comprehensive Pituitary Program was developed as a multidisciplinary effort including the disciplines of Neuro-Endocrinology, Neurosurgery, Radiation Oncology, Neuro-ophthalmology, Neuro-oncology, and Neuro-radiology to coordinate the care of patients with a broad array of Neuroendocrine pathology.
Multidisciplinary Thyroid Nodule and Neoplasm Clinic
The Multidisciplinary Thyroid Nodule and Neoplasm clinic coordinates the efforts among Endocrinologists, Surgical specialists, Radiation Oncologists, Cytopathologists, and Oncologists focused on the care of patients with thyroid nodules and neoplasms.
The program launched the first use of radiofrequency ablation for benign thyroid nodules in Washington State in 2022.
Adolescent and Young Adult Diabetes Program
In 2015, the UW Adolescent and Young Adult (AYA) Diabetes Program was established. Funded by philanthropy and founded jointly by the division and Seattle Children’s Hospital, the clinic is one of the first of its kind on the west coast.
The AYA program addresses the unique health needs of patients transitioning from pediatric to adult diabetes care, a time when patients are particularly vulnerable and may have gaps in care with long-term, devastating consequences.
LatinX Diabetes Institute
In 2020, as part of the UW Medicine Diabetes Institute, the LatinX Diabetes Clinic was launched with the goal of addressing healthcare disparities in LatinX patients with diabetes and addressing cultural and linguistic barriers to high-quality care for this underserved population.
RESEARCH
Our faculty have a long and distinguished history of cutting-edge research, spanning the range of basic science research, through clinical investigation and state-of-the-art innovative clinical care.
The Diabetes Research Center (DRC) supports diabetes research across the University system. It is currently in its 46th year of continuous NIH funding.
Since the inception of the UW DRC Pilot and Feasibility Program in 1977, 92 early-career faculty have been funded and nearly 80% of them subsequently obtained major external funding based on these awards.
The NW Lipid Research Clinic was established in the early 1970s with a dual goal of optimizing clinical treatment of complex lipid disorders and furthering our understanding of the relationship between cardiovascular disease and lipids and the impact of lipid lowering therapies on health.
Over the last 50 years the NW Lipid Clinic has been at the forefront of advances in diagnosis and clinical management of lipid disorders with an overall emphasis on disease prevention.
Today, the NW Lipid Clinic resides at South Lake Union as part of the multidisciplinary care offered at the UW Medicine Diabetes Institute where internationally known researchers and clinicians continue these traditions of excellence.
Type-1 Diabetes
In 2008 investigators at UW reported work in the first randomized controlled trial for continuous glucose monitoring for type 1 diabetes. These investigators play a pivotal role in the 2010s in developing the first hybrid closed-loop automated insulin delivery systems.
 In 2022, researchers found that a pocket-size wearable device known as a bionic pancreas, which uses next-generation technology to automatically deliver insulin, was more effective at maintaining blood glucose (sugar) levels within the normal range than standard-of-care management among people with type 1 diabetes.
In 2022, researchers found that a pocket-size wearable device known as a bionic pancreas, which uses next-generation technology to automatically deliver insulin, was more effective at maintaining blood glucose (sugar) levels within the normal range than standard-of-care management among people with type 1 diabetes.
The leading cause of death for persons with diabetes is cardiovascular disease. Recently, our researchers described apolipoprotein C3, a lipoprotein-associated protein, as both a biomarker and a mediator of cardiovascular disease associated with type 1 diabetes.
These findings highlight new aspects of lipid metabolism as being important in mediating cardiovascular disease risk in people with type 1 diabetes.
Type-2 Diabetes
Basic science studies performed by investigators at UW, including genetic studies, have advanced our understanding of the role of pancreatic beta-cell loss and dysfunction in type 2 diabetes, and are expected to open the avenue for new therapeutic approaches.
Human studies elucidated the critical importance of accounting for insulin sensitivity in interpreting pancreatic beta-cell function, which has been instrumental in the universal acceptance of the critical nature of the pancreatic beta-cell in the development of prediabetes and type 2 diabetes (1990-2010).
Obesity
Similar to the Diabetes Research Center, the Nutrition and Obesity Research Center (NORC) has received over 40 years of NIH funding, supporting research in obesity across the UW and particularly at the UWMDI. Work supported by the NORC has led to many advancements in our understanding of the mechanisms of metabolic diseases.
Research in our division over the last decade has made pivotal discoveries demonstrating that the brain, and in particular the hypothalamus, plays a pivotal role in the development of obesity and insulin resistance.
These insights suggest that new therapies targeting neurocircuitry could be fundamental in overcoming the obesity epidemic.
Male Contraception
For the last 5 decades, the University of Washington has been a leader in work aimed to develop effective, reversible male hormonal contraceptives.
In 2010, UW became one of two sites selected to lead the NIH-funded Male Contraceptive Clinical Trials Network (CCTN).
 In 2019, the first efficacy study of a self-administered male hormonal contraceptive was launched, led by investigators at UW, the Lundquist Institute, NICHD, and the Population Council.
In 2019, the first efficacy study of a self-administered male hormonal contraceptive was launched, led by investigators at UW, the Lundquist Institute, NICHD, and the Population Council.
The study, currently underway at 17 sites across the globe, is also the first male contraceptive efficacy study to include sites in Africa.
This study could lead to the approval of the first reversible, novel male contraceptive to reach the market in over 300 years (the last one being the condom!)
Leadership