Heart-failure deaths surging after a decade of decline
A decade of progressively fewer heart failure deaths in the United States reversed course in 2012. By 2021, heart-failure deaths had rebounded so sharply that they eclipsed the volume of those deaths seen in 1999.
Dr. April Stempien-Otero, associate professor (Cardiology) and a heart-failure specialist with UW Medicine in Seattle, expressed dismay at the data, recently reported in JAMA Cardiology.
“We’d made great progress, and it is really because of these medications we had for heart failure that were revolutionary,” she said. “This uptick … is really surprising and worrisome.”
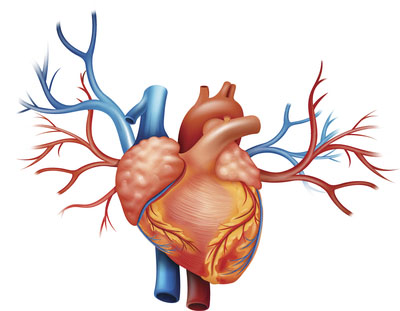
Heart failure occurs when the heart muscle, for a myriad of reasons, cannot pump blood adequately to the rest of the body. The condition causes fatigue, shortness of breath and fluid retention. Medications, however, can improve heart function, decrease symptoms and prolong lives.
“Traditionally we've thought of heart failure as a disease of older people — that, over a long period of time with high blood pressure or disease of the coronary arteries (or) heart attacks, their hearts get weaker. However, this study was interesting because at all age groups, even people below the age of 40, there's increasing risk of heart failure death,” Stempien-Otero said.
The data beg the question of what is causing the resurgence, seen across every demographic stratified by age, sex, race/ethnicity, community size and region.
In parallel to the time span of the study were increases in contributing conditions, such as high blood pressure, diabetes, obesity and increased use of methamphetamines and other addictive toxins. The steeper increases in heart-failure mortality seen in 2020 and 2021 “indicate that the pandemic may have accelerated them,” the authors wrote.
“In addition, we know that the number of patients on the medications that are helpful to treat heart failure has decreased over time,” Stempien-Otero said. “So whereas in 2008, approximately 85 to 90% of patients with heart failure were on our top medication, now it's down to 67%. So people with heart failure are not getting the medications that we know will benefit them.”
Another potential contributor is worse population-level access to healthcare. Stempien-Otero said she and fellow cardiologists wonder if people are not getting primary-care visits that would help reduce risk factors like high blood pressure, diabetes and inactivity.