Division Spotlight: Nephrology
Celebrating 75 years
As part of our 75th Anniversary, we plan to spotlight each of our divisions over the course of the year, in the order that they were established. Learn more about our 75th Anniversary on our website
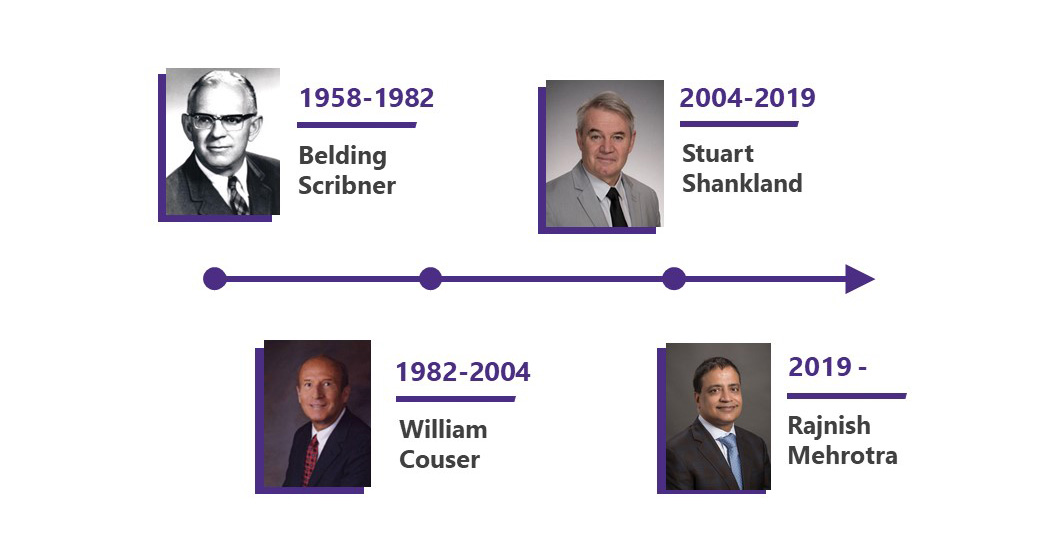
The Division of Nephrology was established in 1958 with the recruitment of Dr. Belding H. Scribner from the Mayo Clinic to the University of Washington.
Since its inception, the division has been known worldwide for bringing innovative solutions to vexing problems. Up through the 1950s, kidney failure was a fatal condition as neither long-term dialysis nor kidney transplantation were feasible treatment options.
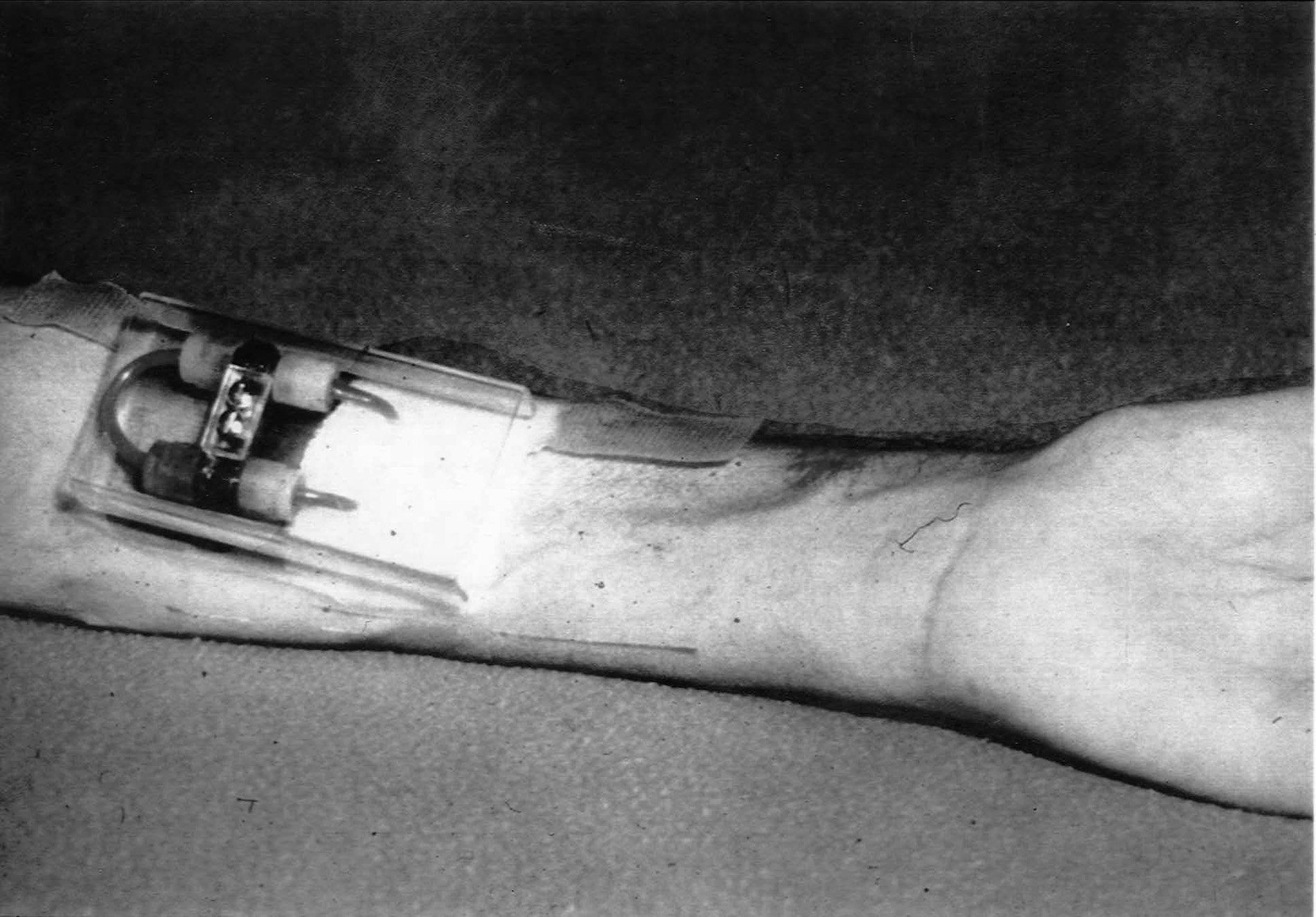
In 1960, Scribner and Quinton developed a blood access device for hemodialysis called the Scribner Shunt, overcoming a critical barrier that finally made long-term hemodialysis possible.
Scribner then worked with the King County Medical Society to establish what is now called the Northwest Kidney Centers in 1962, as the first outpatient dialysis facility in the world.
However, hemodialysis remained a scarce resource through the 1960s, and treatment was available only to people selected for dialysis by the “Life or Death Committee”, which laid the foundation for modern bioethics.

During this period, Dr. Henry Tenckhoff introduced an indwelling peritoneal dialysis catheter that remains the most widely used catheter to date and bears his name.
To maximize the access to lifesaving therapies, Scribner also worked tirelessly with colleagues nationwide to persuade the US Congress to enact the only disease-specific coverage by Medicare in 1973 that has forever changed the clinical practice of nephrology.
Over the past 65 years, divisional faculty have continued to lead and have shaped the field of nephrology – they have included three Presidents of the American Society of Nephrology (Scribner, Couser, Himmelfarb), one President (Couser) and one Secretary-Treasurer (Shankland) of the International Society of Nephrology, Editors-in-Chief of leading nephrology journals (Journal of the American Society of Nephrology: Couser, Mehrotra; Clinical Journal of the American Society of Nephrology: Mehrotra), members of the American Society of Clinical Investigation (current faculty include Shankland, Kestenbaum, de Boer, Bansal) and American Association of Professors (Shankland) and recipients of lifetime achievement awards (Couser, Himmelfarb, Mehrotra, Tuttle), mid-career awards (Bansal, de Boer, O'Hare, Watnick), and early career awards (Duffield, Freedman, Johnson) by nephrology professional societies.
The impact of the work done within the division is further underscored by the American Society of Nephrology conferring the Scribner Award, named after the first division head, to one or more individuals who have made outstanding contributions that have a direct impact on the care of patients with kidney diseases or have substantially changed the clinical practice of nephrology.
Education
We are committed to training the next generation of leaders in the field, to continue to advance clinical care, research, and innovation in the field. The training program further enables residents and medical students to work with nephrology fellows and faculty to further their understanding of the prevention and treatment of kidney diseases.

The Director of Nephrology Education (Dr. Nisha Bansal) oversees and coordinates the different aspects of the educational mission within nephrology (clinical and research) and outside nephrology (medical students, residents, and other trainees).
Our clinical and research trainees have had a major impact on nephrology nationally and internationally and include at least ten nephrology division heads, five Deans of medical schools, and five presidents of national and international nephrology societies.
Nephrology educators have also repeatedly been recognized by medical students (Ryan) and residents (Haseley) as outstanding teachers, and a divisional faculty (Ryan) helped overhaul the medical school curriculum for the first time in 30 years.
Clinical Training
The highly competitive general nephrology fellowship program has been accredited by the ACGME since 1983 and it has trained many of the leaders in the field nationwide. Further, a large proportion of the nephrologists currently practicing in the Pacific Northwest have trained at the University of Washington.
The program recruits 5-6 fellows every year, which includes up to two in the research track. The three clinical sites (Harborview Medical Center, University of Washington Medical Center, and Puget Sound VA) provide our trainees with a diverse population of patients that span the entire spectrum of the specialty, which is further complemented by experience in outpatient dialysis at the Northwest Kidney Centers.

Our trainees diversify their training through extensive subspecialty experience, diverse clinic populations, formal didactics and tutorials, and mentored scholarly activities in a variety of areas ranging from glomerular diseases to home dialysis, and innovative dialysis technologies. Since 2022, the fellows elect one of their second-year peers as the Fleet Chief Fellow.
In addition to general nephrology, the division also provides further subspecialty training within the field. We offer a one-year clinical transplant fellowship, accredited by the American Society of Transplantation. The training spans the entire spectrum of the practice of transplant nephrology, inpatient and outpatient kidney care for all solid organ transplants, education, and patient-centered research. Our program also offers a third year of subspecialty training in dialysis generally or home dialysis specifically, and glomerular diseases.
Research Training
Training in kidney-disease-related research has been supported by an NIH-funded T32 program since 1985 and has been led serially by Couser, Shankland, Shankland/Himmelfarb, and Bansal/Kestenbaum. We recruit up to two fellows on the research track every year and they begin their research training supported by the T32 grant after one year of clinical training.
Research fellows complete at least two years of dedicated research training in clinical, basic, or translational sciences and many trainees successfully compete for additional funding support to bridge their transition to mentored career development grants (K-grants or equivalent). The program has a strong record of success in training physician-scientists in nephrology and a much higher proportion of trainees succeed in procuring career development grants than nationwide.

In 2020, we were fortunate to have received philanthropic support from the Mount Baker Foundation to increase the diversity of research trainees in nephrology. To date, the program has provided support to two nephrology fellows (Limonte, Bullock), and we anticipate expanding the support trainees at earlier stages of training and to non-physicians.
Clinical care
We serve a diverse patient population across the Puget Sound area and with a broad referral from the five-state WWAMI region.
Inpatient Care
Our faculty provide consultative kidney care at three hospitals in the region (Harborview Medical Center, University of Washington Medical Center, and VA Puget Sound) through seven clinical services.
In addition to inpatient general nephrology and transplant care, it includes innovative multidisciplinary team care through the Kidney-Liver program (since 2016) and the Kidney Heart Service (since 2020) at the University of Washington Medical Center.
Illustrative of the high volume of clinical care, in 2022 our faculty provided nearly 15,000 inpatient dialysis treatments and about 170 kidney biopsies.
Outpatient Care
Most of the kidney-disease care is delivered in the outpatient setting and in 2022 we provided ambulatory care with over 25,000 patient-care visits. A large part of this care was delivered through general nephrology clinics at the three primary clinical sites (Harborview, UWMC, VA Puget Sound) and a VA satellite clinic in American Lake.
Over the last decade, we have established at least 13 different subspecialty clinics to provide state-of-the-art clinical care to an increasingly complex population of patients.
This has included Kidney Genetics Clinic and Hypertension Clinic at Harborview Medical Center, Glomerular Clinic, Kidney-Liver, Kidney-Heart, and Onconephrology Clinic at UWMC-Montlake, Kidney Stone Clinic at UWMC-Northwest, Low GFR Clinic at the Puget Sound VA, Transplant-Cancer Clinic at Fred Hutchinson Cancer Center, and Pediatrics-Adult Transplant Transition Clinic at Seattle Children's Hospital.
Further, one nephrologist is embedded within the Diabetes Clinic at South Lake Union, allowing for a multidisciplinary continuum of care at one site.
Kidney Transplant Program
The nationally acclaimed transplant program is the largest in the Pacific Northwest and over 200 deceased and living-donor kidney transplants are being performed at UWMC yearly.
The program is a model of multidisciplinary collaboration and is consistently ranked at or near the top nationally for the time it takes from listing to receiving a transplant and allograft survival. We anticipate continued programmatic growth with the recent establishment of the Transplant Institute.
Outpatient Dialysis Program
We provide outpatient dialysis care to patients in King, Snohomish, and Pierce counties, and include care for patients undergoing in-center hemodialysis or home dialysis (peritoneal or home hemodialysis).
Our care philosophy is highly patient-centered – unique in our community, our nephrology care providers drive to dialysis units to see patients while they are undergoing in-center hemodialysis rather than asking them to drive to our clinical sites during their dialysis-free time. Further, a larger proportion of our patients are treated with home dialysis than in the community or nation at large.
Finally, work at UW has led to the establishment of the first-ever community-based kidney supportive care program at the Northwest Kidney Centers to deliver palliative care to patients undergoing long-term dialysis.
Research
From the time of inception, the division of nephrology has led the field with innovation and discovery. Work done in the early years made long-term outpatient dialysis for kidney failure a reality. Subsequently, under the leadership of Dr. William Couser, UW became the first academic division to focus on understanding the pathogenesis of kidney diseases, particularly immune-mediated glomerular diseases, instead of renal physiology.

Dr. Stuart Shankland further cemented the research credentials of the division with the establishment of the Kidney Research Institute in 2008 with generous support from the Northwest Kidney Centers under the stewardship of the organization’s CEO, Joyce Jackson.
Today, the divisional faculty lead a large and diverse research portfolio that is advancing our understanding of kidney diseases through laboratory research and clinical research that includes translational studies, qualitative research, cohort studies, and clinical trials.
Kidney Research Institute

In 2008, Dr. Jonathan Himmelfarb was recruited as the founding Director of the Kidney Research Institute (KRI), and Dr. Ian de Boer assumed the role in 2022.
The KRI is a collaboration between UW Medicine and Northwest Kidney Centers, and it has catalyzed kidney-disease-related research at UW, across the divisions within the department, across departments within the School of Medicine, and across various schools at UW. Since its inception, the KRI investigators have procured over $200 million in extramural research funding (primarily federal), enrolled over 8000 patients with kidney diseases in research studies, and generated over 1500 original research publications.
Today, the KRI is the central hub of the ambitious NIDDK-sponsored Kidney Precision Medicine Project led by Dr. Himmelfarb. The KRI 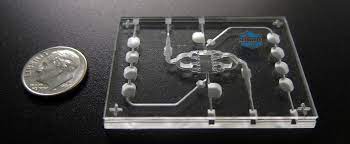 has led the work on “kidney-on-a-chip” as a part of the larger nationwide initiative of “organs-on-a-chip” to accelerate the pace of the discovery of therapeutics.
has led the work on “kidney-on-a-chip” as a part of the larger nationwide initiative of “organs-on-a-chip” to accelerate the pace of the discovery of therapeutics.
There are over 40 investigator-initiated studies ongoing within the KRI that include several clinical trials to advance blood pressure and symptom management and treat secondary hyperparathyroidism in patients undergoing long-term dialysis, depression management in patients with advanced kidney disease, innovative treatments for various glomerular diseases; cohort studies to examine glycemia in patients undergoing long-term dialysis and optimal use of biomarkers for kidney disease in heart failure; translational studies to study tubular function in kidney diseases and autophagy in diabetic kidney disease; and qualitative studies to operationalize non-dialytic management of kidney failure and increase patient-centeredness of transplant evaluation for older adults.

The KRI has led the nation in patient engagement to set the research agenda for nephrology research with the establishment of the Patient Advisory Committee in 2016 and the appointment of a Director for Patient Engagement in 2018.
Today, many of the research studies are guided by patient partners that serve to enhance the meaningfulness of research undertaken by the KRI investigators.
Center for Dialysis Innovation
The Center for Dialysis Innovation (CDI) was established in partnership with UW Department of Bioengineering, with generous funding support from the Northwest Kidney Centers, to develop and test novel and innovative dialysis technologies and to align these technologies with what matters most to patients.
In its view, the ideal solutions would combine the optimization of dialysis therapy with enhanced opportunities for patient independence and autonomy in self-care.
The multidisciplinary team at CDI has expertise in uremia, biomaterials engineering, clinical trials in dialysis, laboratory assays of uremic toxicity, renal nutrition and metabolism, hemostasis and thrombosis, innate immunity, quantitative modeling, vascular access, and patient-centered and health services research.
Laboratory Research
Divisional faculty continue to advance the understanding of the pathophysiology of kidney diseases with laboratory-based research that is broadly based on studying the role of podocytes in glomerular disease and the process of aging in the kidney (Shankland) and using tissue organoids (Freedman).
Both these UW investigators are a part of the NIH-funded (Re) Building the Kidney consortium, to leverage tissue regeneration as a treatment for kidney diseases. Organoids are an innovative approach to understanding disease pathophysiology and the current focus at UW is to advance the understanding of polycystic kidney disease and cystinosis, among others.
Transplantation Research
There is a robust research program that offers transplant recipients state-of-the-art treatments by participating in a large number of ongoing multicenter clinical trials.
Further, the Center for Innovations in Cancer and Transplant (CICT) has recently been established to integrate healthcare and research to transform the lives of people with cancer and organ transplants.
Leadership