Division Spotlight: Cardiology
Celebrating 75 years
As part of our 75th Anniversary, we plan to spotlight each of our divisions over the course of the year, in the order that they were established. Learn more about our 75th Anniversary on our website
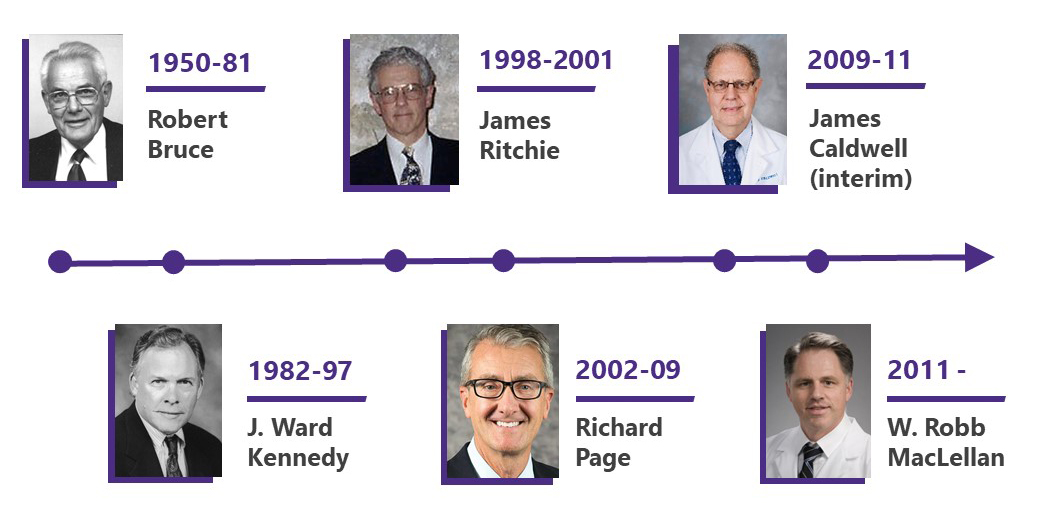
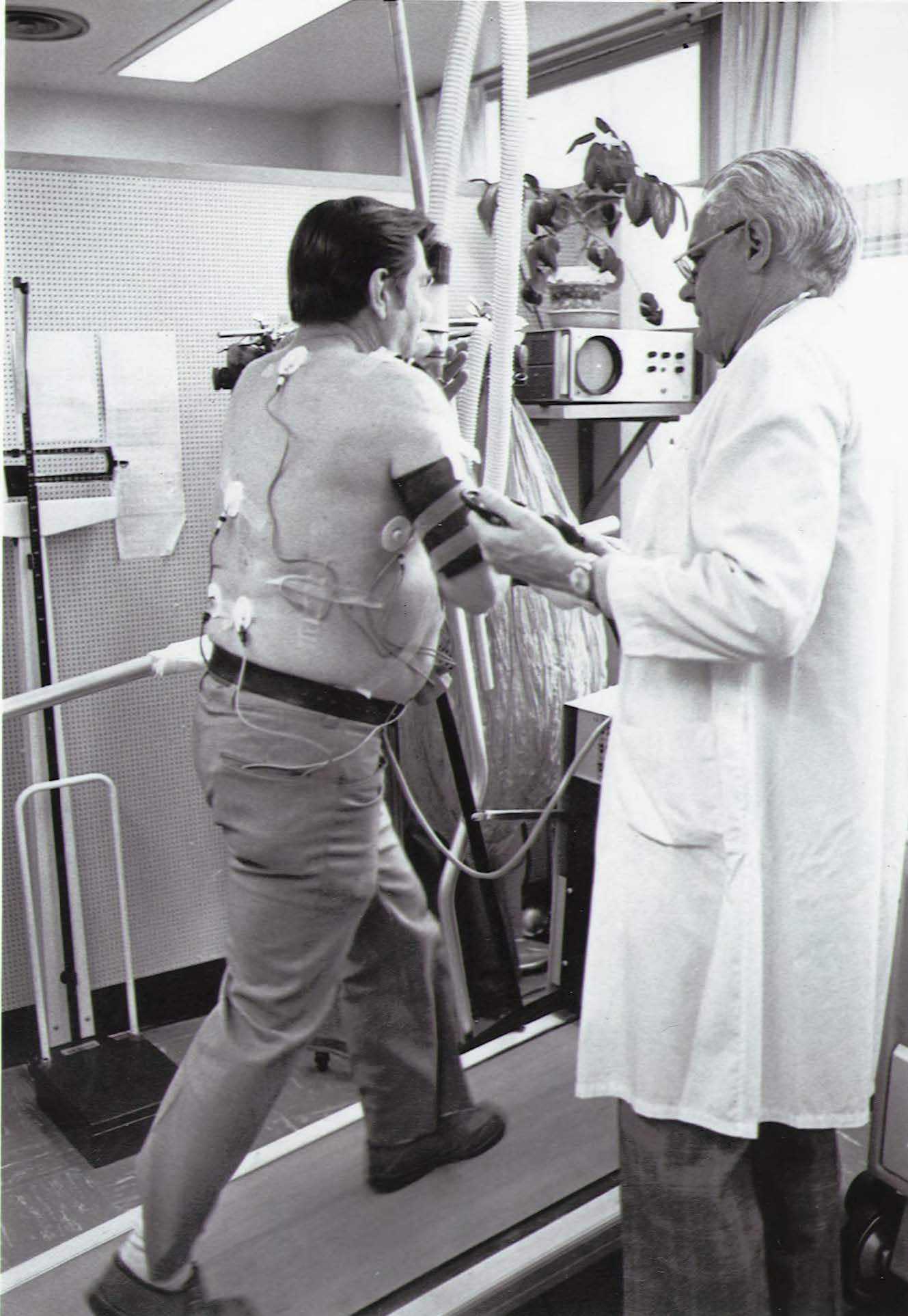
The Division of Cardiology was founded in 1950, and its clinical and research lineages are both traced to Dr. Robert A. Bruce, the founding Division Head. Bruce developed the exercise treadmill test that bears his name: the “Bruce Protocol,” which remains the gold standard for evaluating human cardiovascular function in both clinical and research settings.
Our faculty continue to expand Bruce’s legacy by combining world-class clinical care with ground-breaking research that uses clinical, population, and laboratory-based approaches.
EDUCATION AND FELLOWSHIP TRAINING
Our ACGME-accredited Fellowship Training Program in Cardiovascular Diseases (8 fellows matched per year) – with ACGME subspecialty programs in Adult Congenital Heart Disease (1-2 fellows matched per year), Advanced Heart Failure/Transplant Cardiology (2 fellows matched per year), Clinical Cardiac Electrophysiology (1-2 fellows matched per year), Interventional Cardiology (2 fellows matched per year) – is the only cardiology training program in the five-state WWAMI area.
We are responsible for preparing the cardiologists that serve our region. We currently admit eight fellows per year, with a core curriculum of two years of clinical training and a third year in a clinical scholar, clinical educator or research pathway. Currently, 38 fellows are in our programs.
In addition, we have three non-accredited advanced training programs: Advanced Cardiac Imaging, Structural Heart and Valve Interventional, and Complex, High-Risk and Indicated Percutaneous Coronary Interventions and Advanced Hemodynamic Care Fellowship (CHIP).
We are responsible for preparing the cardiologists that serve our region. We currently admit seven fellows per year, with a core curriculum of two years of clinical training and a third year in a clinical scholar, clinical educator or research pathway. Currently, 38 fellows are in our programs.
Special areas of expertise in our fellowship program include vascular biology, cardiac intervention, echocardiography, electrophysiology, heart failure and cardiac transplantation, new imaging procedures, bioengineering, health services, and clinical trials.
The Cardiovascular Research Training Program supports research training at the interface of discovery and the clinic and provides salary support for 6 postdoctoral trainees. Graduates of the program are well equipped to develop careers as independent investigators in the area of cardiovascular disease.
PATIENT CARE
The Division of Cardiology provides the best of cardiac care, in the hospital and in the community.
The Heart Institute (formerly Regional Heart Center) was created in 2000, combining the divisions of Cardiology, Cardiothoracic Surgery, and Cardiac Anesthesia into a patient-focused clinical service line.
The Heart Institute – providing care at UW Medical Center, Harborview Medical Center, Northwest Hospital, Valley Medical and community clinics – is a common front door for the entire continuum of cardiovascular care, from treadmill tests to transplantation.
The centralized, patient-oriented model of care at the Heart Center allows for seamless integration of services; collegial interaction among physicians; a premier training environment; convenience for referring physicians; and—most important—comfort and ease of access for patients.
Pioneering clinical procedures
Artificial Intelligence
Using smart speakers, a team of researchers developed the first AI system for contactless monitoring of heart rhythms.
BASILICA
We performed a first-in-the-world intentional cut of the aortic valve via catheter to restore function after percutaneous valve replacement. The new technique was named BASILICA: Bioprosthetic Aortic Scallop Intentional Laceration to prevent Iatrogenic Coronary Artery obstruction.
Dissolving stents
The Regional Heart Center was the first cardiology program in Washington state to implant a dissolving coronary stent, implanting the device (which dissolves in three years) in two patients in the first week after the device was approved by the FDA.
Endovascular retrieval system
Interventional cardiologists at the UW Medicine Heart Institute performed a first-in-human procedure, successfully employing a catheter-delivered device to retrieve a benign tumor from inside a patient’s heart.
Micra pacemakers
We implanted the first Micra pacemaker in Washington state. Micra is the world’s smallest pacemaker, less than the size of a AAA battery, and has no wires.
Mitral Valve Repair Therapy
MitraClip Transcatheter Mitral Valve Repair therapy offers a significant treatment advance using a less-invasive and catheter-based approach to repair the mitral valve.
Leveraging a collaborative effort across cardiology, cardiac anesthesia and CT surgery has enabled the University of Washington to become one of the top five sites providing this unique therapy in the U.S.
TAVR
We were one of the very first sites in the United States and the first in the Pacific Northwest to perform transcatheter aortic valve replacement (TAVR).
Total artificial heart
We were the first in the Pacific Northwest to discharge a patient with a total artificial heart. In the past, patients would need to remain in the hospital until they received a transplant but with this new piece of technology – called the freedom driver – they can be discharged.
Our patient was the first in the Northwest and one of only 25 to have ever received the artificial heart, equipped with the freedom driver, in the country.
RESEARCH
Research related to cardiovascular health takes place across a range of specialties in the department, reflecting the many risk factors and manifestations of disease, as well as the spectrum of treatment modalities. Patient-centered investigation with direct applications to clinical care is a high priority.
Our faculty and staff carry out laboratory-based, clinical, and population-based research. Our projects are aimed at understanding the causes of cardiovascular diseases, evaluating current therapies, developing new therapies, and designing preventive strategies.
Research projects cover a broad spectrum, including: studies that elucidate the fundamental biology of the heart and blood vessels; investigations that uncover mechanisms of cardiovascular diseases; and preclinical as well as clinical trials of new therapies for diseases such as atherosclerosis, arrhythmias, heart failure, congenital cardiovascular disease, and valvular heart disease.
Heart Regeneration Program
We are using stem cell technology to repair the heart. By injecting heart cells made from stem cells into the heart of patients awaiting heart transplants, we can look at the damaged organ after the patient gets a new heart, to see if the stem cells helped regenerate the heart muscle tissue.
Cardiovascular Health Research Unit
The Cardiovascular Health Research Unit (CHRU) is a joint program of the UW’s Department of Medicine, Divisions of Cardiology and General Internal Medicine, and the Group Health Research Institute.
CHRU investigators conduct epidemiologic and health-services research addressing cardiovascular disease risk factors, prevention, and treatment, including genetic studies of sudden cardiac arrest and resuscitation outcomes.
Center for Cardiovascular Innovation
The Center for Cardiovascular Innovation is focused on accelerating the development of cardiovascular devices for the diagnosis and treatment of coronary and peripheral artery disease, structural heart disease, heart failure and heart rhythm disorders.
Clinical trials
Our Clinical Trials Unit supports biomedical research endeavors to improve heart and vascular health outcomes.
Global cardiology
Cardiovascular diseases (CVD), including heart diseases and stroke, account for one-third of deaths throughout the world. At the Institute for Health Metrics and Evaluation, we are leading cardiovascular disease modeling for the Global Burden of Disease Study.
In 2021, we partnered with the Department of Global Health to create a joint Global Cardiovascular Health Program dedicated to global cardiovascular disease prevention and care.
Resuscitation outcomes
We are testing new kinds of intravenous solutions, the roles of CPR and shock, and other approaches to improving resuscitation, and local efforts to improve cardiac resuscitation outcomes through innovative technology, methods, and training.
Seattle Proportional Risk Model
Sudden death is involved in one-half of all deaths in patients with chronic heart failure. An implantable cardioverter-defibrillator (ICD) can decrease sudden death by 60 percent.
Our researchers have developed the Seattle Proportional Risk Model (SPRM) to identify which heart failure patients are at greater risk of sudden death, and more likely to benefit from an ICD.
Sports Cardiology
The University of Washington Center for Sports Cardiology offers exceptional clinical care, expand research and educational programs, and accelerate needed advances in the cardiovascular care of athletes.
Leadership