Breaking boundaries for better aortic care
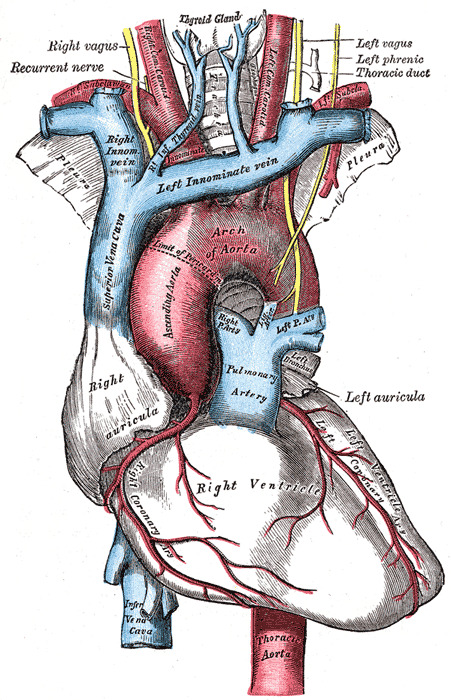
The aorta is the biggest artery in the body. This cane-shaped vessel carries oxygenated blood not only from the heart to the brain, but also to the abdomen and lower extremities. Because it extends into the body’s upper and lower regions, the aorta crosses into the domains of several different medical specialists, including surgeons, cardiologists and medical geneticists.
From a surgical perspective, conditions affecting the aorta below the diaphragm have traditionally been known as vascular surgeon territory. Cardiac surgeons lead aortic repair around the heart and into the top of the aorta — also known as the aortic arch.
A team at UW Medicine is intentionally breaking down these long-standing care boundaries. They’ve created the Multi-disciplinary Thoracic Aortic Program (MTAP) to provide holistic, team-based care for complex aortic disease.
The beginnings of MTAP
Matthew Sweet, MD, a vascular and endovascular surgeon at UW Medical Center – Montlake, began practicing at UW Medicine 12 years ago. His earliest cases involved placing stents to treat thoracic and abdominal aortic aneurysms.
“I began to see many patients with an aneurysm in the thoracoabdominal area, as well as in the aortic arch,” Sweet says. “Those with an arch aneurysm needed cardiac surgery, so I was hitting a wall with their care. I needed a cardiac surgery partner to manage these cases more collaboratively.”
Around the same time, Christopher Burke, MD — who had completed his training at UW Medicine — returned to campus following a six-month specialty training in arch surgery.
“I’d known Dr. Burke for years, and we both said, ‘Hey, let’s collaborate to take care of these patients who need both of our expertise,’” says Sweet.
But surgery is just one part of aortic disease care. And not all patients need surgical repair. So, Burke and Sweet reached out to other specialists involved in various aspects of care for these complex patients.
With a team of cardiologists, cardiac surgeons, clinic staff, genetic counselors, medical geneticists and vascular surgeons on board, the multidisciplinary team MTAP formed.
Catherine Otto, MD; Yonatan Buber, MD; and James Kirkpatrick, MD, in the Division of Cardiology were instrumental in supporting this effort, along with Peter Byers, MD, a medical geneticist with a wealth of expertise in genetic conditions affecting blood vessels. All have been critical additions to the team, says Sweet.
Over the years, vascular surgeon Sara Zettervall, MD, and cardiothoracic surgeon Scott DeRoo, MD, have become integral surgical partners on the team as well, he adds.
Why collaborative aortic care matters
Sweet says care planning for aortic disease is critical to long-term outcomes. This is especially true for patients at risk for aortic aneurysms due to family history or a genetic disorder, like Marfan syndrome, which affects the body’s connective tissue.
“The way surgeons repair the aorta near the arch can impact surgical options for a later repair of the thoracoabdominal aortic aneurysm,” Sweet says. “A first surgery done a specific way can set up patients for future successful procedures.”
And, adds Burke, because so many patients with complex aortic disease need lifelong care, a coordinated, team approach can make all the difference.
How MTAP works
The team meets weekly to discuss complex aortic disease cases. The patients are later presented with a consultation from their direct provider that comes out of those multidisciplinary discussions.
On any given week, that team exceeds a dozen providers and trainees. Together, they develop short-term and long-term care plans. And — despite MTAP’s founders being surgeons — surgery isn’t always part of the plan.
“We have patients in our clinic with genetic aortopathy,” Sweet says. “They may never need surgery, but we must discuss how we will help them modify their risk factors and monitor them.”
Burke and Sweet say the program is all about making sure patients have the most seamless and effective care without being sent from doctor to doctor for extra or unnecessary testing.
“We connect all the steps in the process for the patients to improve their care and overall experience,” Burke says.
A program unlike any other
Over a year, the MTAP team discusses 250 to 300 patient cases.
“I don’t know any place with the same fluidity of communication, frequency of meetings and collegiality,” Burke says. “‘Aortic center’ has become a buzzword across the country, but there’s no definition. I think that term gets used by institutions with nowhere near the level of organization, commitment and consistency we have here.”
The program’s uniqueness, say Burke and Sweet, benefits both patients and referring providers.
“We have doctors here who are super-specialized within their field and can serve as an outlet for providers in our region and beyond whose patients need treatment for complex aortic problems,” says Burke.
However, the multidisciplinary team also benefits from the program’s collaborative nature.
“The best part of work is having colleagues you enjoy working with and having a forum where you all prioritize making time to talk and think about these things,” Sweet says. “I’ve been a faculty member for 12 years, and MTAP is one of the most exciting things I’ve been a part of.”
Burke agrees.
“What’s so enjoyable about this work is that we all have come together with the mindset of, ‘I can’t do everything, but I can do a few things really, really well. And I can do my work with other people who do other things really, really well,” says Burke. “It’s more than a program that we’ve built. It’s also a new way of doing things — a culture change.”
And the team is expecting a very bright future. They are eyeing a major clinical trial and have the infrastructure to collaborate with industry partners.
“We have all the right people at the table,” Sweet says. “It’s something that others want to be a part of.”