


Vaccination after COVID infection boosts key immune cells
Researchers have found that people who received mRNA vaccines against SARS-CoV-2 after a COVID-19 infection produce a large number of key immune cells.
The finding might explain why people who have acquired immunity against the virus from both natural infection and vaccination — so-called hybrid immunity — are better able to resist reinfection than are those whose immunity stems from either infection or vaccination alone, said Dr. David Koelle, who led the research. He is a UW professor of medicine in the Division of Allergy and Infectious Diseases.
“We found that receiving the standard initial mRNA vaccine two-dose series after having been infected not only boosts memory immune cells acquired during the original infection, but also elicits the production of a diverse population of new cells as well,” Koelle said.
This diversity could help protect against new variants of the virus that may emerge after the first infection, he added.
Dr. Emily Ford, UW assistant professor of of medicine; Koshlan Mayer-Blackwell, senior data scientist at the Fred Hutchinson Cancer Research Center; and Lichen Jing, a research scientist in the Koelle lab, were co-lead authors of the paper, which appeared in Nature Immunology.
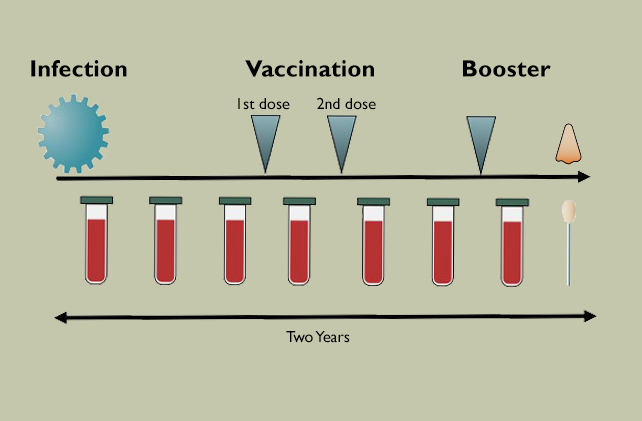
In the study, the researchers followed 53 people who had become infected with SARS-CoV-2 early in the pandemic before vaccines became available. The scientists collected blood samples as the patients recovered from their infections and then again after they received the first two mRNA vaccines and later after a booster. They also took nasal swabs from participants to see whether immune cells were in the respiratory tract lining.
They focused on T cells, in particular CD8 T cells, which play an essential role by directly limiting viral replication.
T cells have proteins on their surfaces, receptors, that bind to portions of foreign proteins. When this happens, the cells begin to proliferate, generating an army of clones that target and destroy infected cells. In the case of SARS-CoV-2 mRNA vaccines, T cells bind to portions of the spike protein that the virus uses to latch onto and invade cells.
The sequences of the T cell receptors vary, so it is possible to identify different clone populations by sequencing their receptor genes. Koelle and his colleagues were able to do this with the help of the Seattle-based biotech company Adaptive Biotechnologies, which donated its sequencing services for the project.
Using these sequences as a kind of barcode for each CD8 T cell clone, the researchers were able to determine that, as expected, the number of CD8 T cells that had been generated in response to the initial infection fell as immunity waned.
With vaccination, however, the number of CD8 T cells targeting the spike protein jumped. This was partly due to the activation of clones descended from the CD8 T cells generated during the initial infection, called memory T cells. In addition, the researchers detected the emergence of large numbers of new clones bearing T-cell receptors with previously unseen sequences.
“This indicates that receiving an mRNA vaccine after infection not only boosts the numbers of the memory immune cells acquired during the original infection, but also elicits the production of a diverse population of new clones,” Koelle said.
He added that such T cell diversity might explain why hybrid immunity can protect against reinfection by new viral variants, which typically have changes in spike proteins that help them elude antibodies generated by prior infection.
The fact that CD8 cells numbers and diversity jumped after the mRNA vaccination is important for vaccine development because CD8 cells do not respond to many currently available types of vaccines, according to Koelle.
“Researchers in the vaccine field have been looking for ways to elicit potent CD8 T cell response for many years,” he said. “Currently only live virus vaccines such as measles, mumps and rubella and the oral polio vaccines have been able to do that. But they, being live, raise safety concerns and are expensive to make. Now, we have documented that these mRNA vaccines, which are relatively cheap and are flexible, are good CD8 boosters.”
Nasal swabs conducted at the end of the study found that CD8 T cells had migrated to the nasal mucosa, where, by defending the tissue through which the virus most often enters the body, they likely confer added protection against reinfection, Koelle said.
This work was supported by the U.S. National Institutes of Health, National Institute for Allergy and Infectious Diseases and the Department of Health and Human Services: 75N93019C00063, AI163999, K08 446 AI148588, R01 AI136514, F30 CA254168, T32 CA080416, 447 P01 CA225517, R01 AI134878, UM1 448 AI068614, HHSN272201800013C. The scientific computing infrastructure at Fred Hutchinson Cancer Center was funded by the National Institutes of Health Office of Research Infrastructure Programs: (S10 OD028685).