Division Spotlight: Rheumatology
Celebrating 75 years
As part of our 75th Anniversary, we plan to spotlight each of our divisions over the course of the year, in the order that they were established. Learn more about our 75th Anniversary on our website
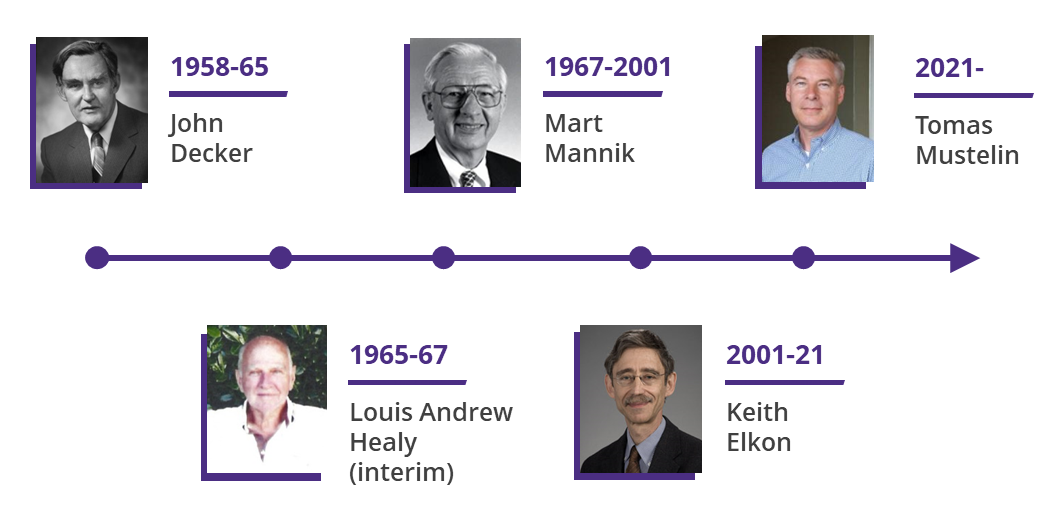
Originally named the Division of Arthritis, the Division of Rheumatology was founded in 1958 by Dr. John Decker and consisted of him and one other faculty member. The Division grew slowly at first, then accelerated under Dr. Mart Mannik’s leadership 1967-2001, and then tripled in size under Dr. Keith Elkon, who led the Division from 2001–2021.
Today, the Division is led by Dr. Tomas Mustelin and consists of 32 faculty members, with active recruitment underway. Our family also includes a vibrant group of teaching associates, fellows, post docs, volunteers, and research and administrative staff. Our faculty are national leaders in the care of rheumatic conditions, in basic, translational, and clinical research, and in training future leaders in rheumatology.
EDUCATION AND FELLOWSHIP TRAINING
Fellowship
Founded in 1967, our Rheumatology Fellowship Program is nationally recognized as one of the longest-running NIH-funded programs in the country. We still celebrate our first fellow, Dr. James Lane, with the annual endowed Lane Lecture, given by an internationally influential and eminent speaker.
Our 2-year fellowship program offers world-class and highly individualized training for the next generation of rheumatology researchers, clinicians and educators. With 4 new fellows each year, we are now one of the largest rheumatology fellowship programs in the US.
Fellows work closely with expert clinicians at four mission-driven Seattle hospitals to develop comprehensive clinical skills and knowledge. Those interested in pursuing research-oriented careers as independent investigators are supported by highly experienced mentors at UW and allied research institutes.
Clinically-oriented fellows are also involved in research and scholarship but receive additional training for careers in academic medicine and medical education or rheumatology practice in the community, particularly underserved areas in the 5-state Washington, Wyoming, Alaska, Montana and Idaho (WWAMI) region.
Research training
We have held an NIH T32 training program in Adult/Pediatrics Rheumatology that has trained over 120 rheumatologists since its inception in 1975. The goal of our combined adult and pediatric training program is to provide MD and PhD postdoctoral fellows high quality training in rheumatic disease and to equip them to become independent academic researchers.
PATIENT CARE
We care for patients across the full spectrum of rheumatic conditions, with particular areas of expertise including inflammatory arthritis, connective tissue diseases, myopathies, vasculitis, and rare or suspected rheumatologic disease. As a tertiary referral center, we see plenty of complex, difficult to diagnose, and challenging to manage cases.
Inpatient
Four UW Medicine-affiliated medical centers provide inpatient rheumatology services in the greater Seattle area: University of Washington Medical Center-Montlake, University of Washington Medical Center- Northwest, Harborview Medical Center, and VA Puget Sound Health Care System.
Outpatient
Our outpatient services provide broad-spectrum care for rheumatology patients. Our general Rheumatology clinics are available at HMC, VA, and the Rheumatology Clinics at Northwest Outpatient Medical Center and UWMC- Roosevelt. Most of these clinics are teaching clinics, where a medical student, resident, or rheumatology fellow may also participate in patient care.
We also provide subspecialty care in musculoskeletal ultrasound, Dermatology/Rheumatology, Interstitial Lung Disease/Rheumatology, and Neuromuscular Diseases/Rheumatology. Our providers in these subspecialty clinics meet regularly to work collaboratively on patient care to provide full-spectrum, interdisciplinary disease management.
RESEARCH
Our division is a leader within the Department of Medicine in the number of registered innovations and filed and out-licensed patents.
Our faculty’s research is funded by numerous grants from the National Institutes of Health, foundations and the generosity of local donors. Research findings are published regularly in national and international scientific journals. In addition, faculty members have contributed to many textbooks on rheumatology and internal medicine.
Rheumatoid Arthritis
Over the course of our history, our faculty have made numerous discoveries in the treatment and management of rheumatoid arthritis (RA).
Dr. Robert Willkens, a nationally prominent rheumatologist and UW faculty member for 50 years, cared for some of the first patients at Harborview Medical Center and was a pioneer in arthritis research. Beginning in the 1980s he was influential in the use of Methotrexate in to treat RA and published one of the first placebo-controlled studies of its benefit in treating RA.
Additionally, Gordon Starkebaum contributed multiple studies of immune complex interactions with cells and William Arend laid the groundwork for the development of IL-1 inhibitor as a therapeutic protein for the treatment of rheumatoid and other forms of arthritis.
Today, our division is home to several research programs and laboratories dedicated to rheumatoid arthritis, greatly aided by the established Rheumatology Biorepository, which enables the study of patient samples.
Systemic Lupus Erythematosus

Much emphasis has been placed on the disease mechanisms in systemic lupus erythematosus, spearheaded by Dr. Elkon, who has followed his old mentor’s advice of ‘try to solve this lupus thing’.
Dr. Elkon and his colleagues have published numerous studies of immune complexes, circulating DNA, oxidation of DNA, role of mitochondria in autoimmunity and tissue calcification, and biomarkers for rheumatological conditions. In addition, numerous contributions have been made to our understanding of lupus since the 1980s, including the role of autoantibodies, type I interferons, innate immune cell processing and response to dead and dying cells, response to ultraviolet light, and DNA sensing.
Our faculty discovered the PTPN22 risk allele in autoimmunity and led the development of anti-interferon receptor (anifrolumab) approved in the U.S. and Europe by the FDA for the treatment of lupus in 2021, plus several other therapeutics.

Our current lupus researchers Dr. Christian Lood and Dr. Mustelin continue to find new autoantibodies with clinical association, biomarkers, and other disease mechanisms and Dr. Lee Nelson discovered the role for microchimerism in initiating the pathogenic mechanisms of scleroderma and neonatal lupus, SLE, and pediatric scleroderma. We have also published work supporting a role of retrotransposons and endogenous retroviruses in lupus.
Myositis, vasculitis, psoriatic arthritis and other rheumatologic conditions
Current research also focuses on inflammatory myositis and vasculitis, complementing our Fast-Track Clinic in giant cell arteritis (GCA), a rare, but potentially devastating rheumatic emergency. We provide an immediate conduit for the management of this disease, which can lead to sudden blindness if not treated effectively.
Our faculty are interested in many additional rheumatic and autoimmune conditions and played a key role in the development of brodalumab (anti-IL-17 receptor A) approved in the U.S. and Europe for the treatment of psoriasis and psoriatic arthritis in 2017, plus several other therapeutics.
Leadership