Division Spotlight: Pulmonary, Critical Care and Sleep Medicine
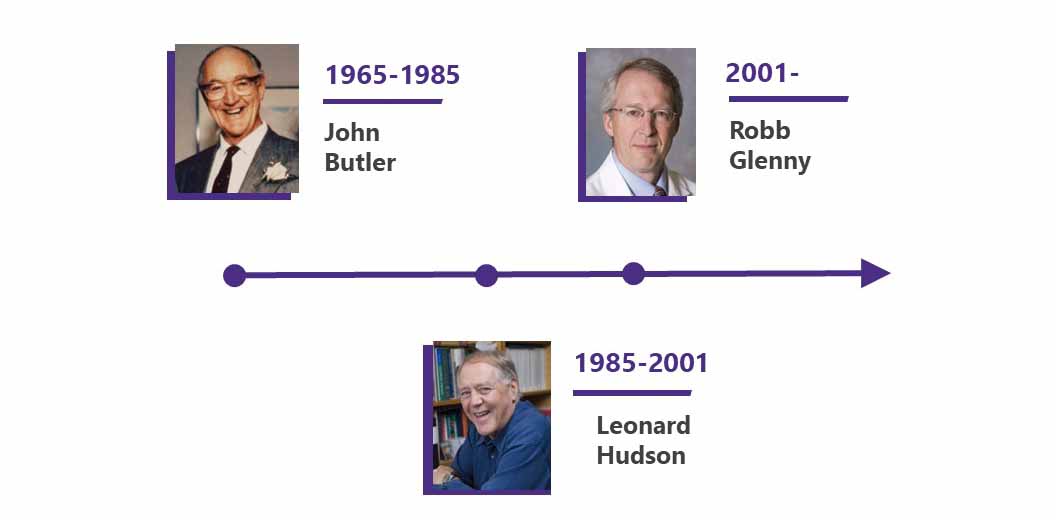
The Division of Respiratory Diseases was founded in 1965 by Dr. John Butler and later renamed the Division of Pulmonary and Critical Care Medicine. Sleep medicine was added to the division name in March 2017.
Celebrating 75 years
As part of our 75th Anniversary, we plan to spotlight each of our divisions over the course of the year, in the order that they were established. Learn more about our 75th Anniversary on our website
Our division is internationally recognized for the rigor and breadth of our training program, clinical expertise, and innovative research.
EDUCATION AND FELLOWSHIP TRAINING
With fellowships in Pulmonary and Critical Care, Sleep Medicine, Critical Care Medicine and Palliative Care Research, the division is recognized both for clinical excellence and commitment to providing a superb clinical training environment.
Continued protection of time for scholarly activity is central to retaining our highly qualified and dedicated clinician educator faculty.
As clinical intensivists, division faculty members provide global support for other medical services throughout the medical centers, allowing other physicians to deliver clinical care to more complicated patients within their own specialties.
As one of the nation’s best clinical training programs, the division has trained the vast majority of the pulmonary and critical care physicians with the Pacific Northwest and WWAMI region.
Graduates of our training program are leaders in our specialty, populating numerous academic Pulmonary and Critical Care Divisions around the country.
We have an exceptionally strong tradition of developing independent physician/scientists. Since the start of our training program, hundreds of fellows have been trained with the vast majority becoming leaders in academic medicine.
These individuals are nationally recognized in their fields of research and actively mentoring the next generation of researchers.
Graduates of our training program are leaders in our specialty, populating numerous academic Pulmonary and Critical Care Divisions around the country, serving in executive positions within professional organizations, participating in NIH study sections, and acting as board members for research foundations.
Our training environment is superb. A third of the faculty members in the division are physician/scientists with focused research projects and extramural funding in one of our broadly categorized research groupings. Two broad tracks have developed under the headings of Pre-Clinical and Clinical Research.
Within the Pre-Clinical track, faculty focus on immunity, lung repair, computational biology, microbiology and physiology.
Within the Clinical track, research encompasses health services, health equity, epidemiology, clinical trials and informatics. Integration of these diverse areas is promoted through translational research projects and a mutually supportive research environment that allows fellows and faculty to continually initiate investigations into new areas.
PATIENT CARE
Division faculty staff the Chest Clinics at Harborview Medical Center, the University of Washington Medical Center (Montlake and Northwest), Fred Hutch Cancer Center and the VA Puget Sound Medical Center.
Patients receive evaluation and education for a wide range of pulmonary and respiratory-related diseases including asthma, emphysema, COPD, lung cancer, sarcoidosis, pulmonary fibrosis, pulmonary hypertension, and cystic fibrosis.
The latest in diagnostic techniques are available in all outpatient clinics, along with smoking cessation assistance, medication management, and social support.
Lung Cancer Early Detection and Prevention
The Lung Cancer Early Detection and Prevention Clinic at Fred Hutch Cancer Center and the Lung Cancer Screening and Nodule Detection program at the VA are unique to the region. These clinics provide careful risk assessment and screening when necessary for lung cancer and other pulmonary diseases in those who have been exposed to smoke or diagnosed with lung nodules.
Lung Transplant Program
UW Medical Center's Lung Transplant Program, in partnership with the VA, is the leading program of its kind in the Pacific Northwest, and one of two programs with the VA system. More than 1,000 lung transplants have been performed at the center, and Department of Medicine pulmonary physicians are central members of the interdisciplinary team caring for transplant patients.
Interdisciplinary Research in Critical Illness
Critical illness is a multi-system disorder. A comprehensive research program targeting critical illness mandates a multidisciplinary approach in which investigators from diverse fields of interest focus their combined skills on the complex interactions of systems that occur in critical illness.
Currently, there is no single entity that brings together multidisciplinary specialists to focus on the problems of critically ill patients.
The division is focusing the remarkable resources of the University of Washington and the Seattle area on improving treatment and outcomes of these patients.
Acute Lung Injury/Acute Respiratory Distress Syndrome
Acute lung injury (ALI) is a condition that causes respiratory failure. Acute respiratory distress syndrome (ARDS) is a more severe form of ALI, one associated with lung injury caused by pneumonia, trauma, bloodstream infections, and other conditions. ALI/ARDS presents a huge medical challenge, especially in intensive care units. The disease affects 190,000 people every year in the United States.
Of those diagnosed with ALI/ARDS, 40 percent of patients die from the condition. At UW Medicine, the division of Pulmonary, Critical Care and Sleep Medicine is researching both the molecular mechanisms behind ALI/ARDS and treatment options for the syndrome.
As part of that work, we participate in a clinical treatment network, funded by the National Institutes of Health that identifies and tests treatments for use in intensive care units. NIH has recognized our division as a Specialized Center of Clinically Oriented Research in acute lung injury.
Palliative Care in the Intensive Care Unit
Harborview Medical Center, one of UW Medicine’s teaching hospitals, houses the Cambia Palliative Care Center of Excellence, an innovative program focused on the study of palliative, or end-of-life, care in the intensive care unit.
Researchers are looking at the way critically ill patients are cared for, investigating how medical caregivers communicate, how patients and families feel about their treatment, and how cultural factors influence ICU care.
The results of these studies are used to design training and education programs for patients and staff throughout the School of Medicine — including the Division of Pulmonary, Critical Care and Sleep Medicine.
Interstitial Lung Disease
Interstitial lung disease causes scars in the lung that eventually make breathing difficult. Patients with interstitial lung disease are hard to treat because they typically face a wide array of complicated medical and respiratory problems.
Through intensive research, locally and through multi-center clinical trials, we hope to create better, more individualized tools to diagnose and treat interstitial lung disease — and to help relieve the suffering associated with this ailment.
Cystic Fibrosis
The University of Washington Medical Center has one of the leading Adult Cystic Fibrosis Centers in the nation. By actively partnering with the pediatric community, researchers and physicians at UW have been significant contributors to advances that allow patients with cystic fibrosis to live into adulthood. Adult patients with cystic fibrosis bring a new set of challenges including different health care and social issues.
COPD
Clinicians within the division treat patients with emphysema and chronic bronchitis with the most current treatments available while clinical researchers at the VA Puget Sound Medical Center focus on identifying and disseminating best practices in caring for patients with chronic obstructive pulmonary diseases (COPD).
Sleep Medicine
Outpatient clinics dedicated to the evaluation and treatment of sleep disorders are established at Harborview Medical Center, the VA Puget Sound Medical Center and the University of Washington Medical Center.
The Sleep Medicine Program is a multidisciplinary effort between the Departments of Medicine, Neurology, Surgery, Psychiatry and Pediatrics. The Program also provides the foundation for one of the country’s best sleep medicine fellowship programs.
Assisted Breathing
Patients suffering from spinal cord injury or neuromuscular weakness that impinges on their ability to breathe are cared for in our Northwest Center of Excellence for Assisted Ventilation and at the VAP Puget Sound Medical Center. We partner with the Department of Rehabilitation to provide care for a population of patients who have unique needs that are not easily met through traditional care providers.
RESEARCH
Prior to COVID-19, lung disease was the third most common cause of mortality in the United States and millions are living with chronic conditions such as asthma, emphysema, cystic fibrosis, and occupational disease.
Understanding the cellular and molecular biology underlying these intractable disorders holds the key to developing novel, effective treatments.
Department of Medicine pulmonologists and other specialists lead both longstanding and newly created approaches to that goal. They are participating in major national programs to improve treatment for some of the most widespread and devastating pulmonary disorders, including acute respiratory distress syndrome (ARDS), acute lung injury (ALI), and chronic obstructive pulmonary disease (COPD).
Our research programs encompass a broad range of interests including cell and molecular biology, integrative physiology, clinical and genetic epidemiology, computational biology, clinical outcomes, and translational research.
Investigators currently hold federally funded and foundation awards at the R01/Merit and career investigator (K and CDA) level. In addition, we have successfully competed for and been awarded multi-project awards such as SCCORs and Program Project grants.
We continue to be active participants in a number of multi-centered NIH-funded clinical trials. The VA Health Service Research and Development (HSR&DF) and the VA Center of Innovation for Veteran-Centered and Value-Driven Care (COIN) provide the foundation of our health outcomes research programs.
This wide variety of research opportunities attracts a large and highly competitive class of fellow trainees to our NIH-supported research training program.
Center for Lung Biology
The Division’s Center for Lung Biology brings together UW scientists, as well as researchers from other institutions, to build cross-disciplinary research programs devoted to understanding lung disease and repair.
The center explores the common mechanisms of pulmonary disease processes, including immunity, inflammation, and repair, conducting research that promises to lead to new and better treatments for lung injury and disease.
In addition to adding to the body of knowledge on pulmonary diseases, such basic research often has wide-reaching implications for other fields of medicine.
Division Leadership